Selecting optimal dental restoration materials poses a significant challenge for modern laboratories and clinicians facing diverse patient needs. Here is the deal: making an incorrect choice often leads towards patient dissatisfaction, costly remakes, and damaged professional reputations that take years building back up. Zirconia crowns and PFM restorations represent two dominant solutions, yet deciding between them requires deep technical knowledge regarding material properties and clinical performance. As experts in zirconium product manufacturing, we provide the insights needed for informed decision-making. By understanding specific advantages inherent in zirconia powder quality and processing, your business can ensure superior outcomes that drive growth and trust.
What Defines Zirconia and PFM Restorations?

Restorative dentistry has witnessed a massive shift in preferred materials over recent decades as technology evolves rapidly. You might be wondering, what exactly distinguishes these two dominant contenders at a fundamental level? Zirconia crowns utilize zirconium dioxide, a crystalline oxide form of zirconium metal that functions as a robust ceramic material. This substance delivers high-strength metal-free solutions for diverse clinical situations ranging from single units to full-arch bridges. It represents a leap forward in material science, offering biocompatibility alongside impressive mechanical resilience.
Porcelain Fused to Metal (PFM) combines a metallic substructure with a layered ceramic veneer to mimic natural dentition. This hybrid approach has served dentistry for over fifty years, offering reliability alongside decent aesthetics for many standard cases. However, modern demands for metal-free dentistry drive a transition toward advanced ceramics that offer better light transmission. Dental laboratories must recognize how raw material quality impacts final restoration success and longevity. Utilizing premium zirconium silicate for glazing or high-purity powders ensures consistent sintering results and structural integrity. Lower grade inputs often result in fractures or poor translucency, compromising a final product before it even reaches the patient.
How Do Material Compositions Differ
Material science serves as a backbone for high-quality dental restorations that must withstand extreme oral environments. But here’s the kicker: atomic structure determines clinical performance and long-term failure rates. Zirconia consists of a polycrystalline lattice, often stabilized with yttria for maintaining a tetragonal phase at room temperature conditions. This “transformation toughening” mechanism prevents crack propagation, making it unique among dental ceramics available today.
PFM restorations rely on a mechanical and chemical bond between a cast or milled metal coping and feldspathic porcelain layers. Alloys range from high-noble gold which offers great fit, to base metals like nickel-chromium which reduce cost but increase allergy risks. Achieving a chemical bond between metal oxides and opaque porcelain requires precise thermal management during firing cycles.
Choosing correct zirconia ceramic structural parts partners remains crucial for labs producing zirconia discs or custom abutments. Consistent particle size distribution in raw powder directly influences density and shrinkage rates during sintering processes. Inconsistent materials lead toward ill-fitting crowns requiring manual adjustment, increasing labor costs significantly for a lab business.
| Feature | Zirconia (Y-TZP) | PFM (Base/Noble Metal) | |
|---|---|---|---|
| Core Material | Zirconium Dioxide | Metal Alloy (Ni-Cr, Co-Cr, Au) | |
| Veneer | Monolithic or Layered Porcelain | Feldspathic Porcelain | |
| Flexural Strength | 900 – 1400 MPa | Metal: >1000 MPa, Ceramic: ~100 MPa | |
| Thermal Conductivity | Low | High (Metal transfers heat) | |
| Biocompatibility | Excellent | Varies (Nickel allergy risk) |
Which Option Offers Superior Aesthetics?

Aesthetics often drive patient acceptance for anterior restorations where visibility remains high. What’s the real story? PFM crowns historically struggled with light transmission due largely to their opaque metal core blocking all light. This metal substructure necessitates an opaque porcelain layer that can make teeth look flat or lifeless in natural lighting. Furthermore, gum recession often reveals a dark metal collar, creating an unsightly “black line” at gingival margins which patients despise.
Zirconia overcomes these hurdles through inherent translucency and white coloration. Modern high-translucency (HT) zirconia allows light passage through a restoration similar to natural dentin layers. Even monolithic crowns now offer graded shading mimicking natural tooth structure from cervical to incisal areas without needing external stain.
For maximum aesthetic results, technicians apply specialized porcelain powders over a zirconia core to create depth. This layering technique provides vitality without risking dark margins associated with metal substructures. Laboratories prioritizing aesthetic excellence find zirconia offers greater versatility for demanding cases requiring perfect shade matching. Sourcing high-quality Zirconia discs enables technicians to achieve these results consistently.
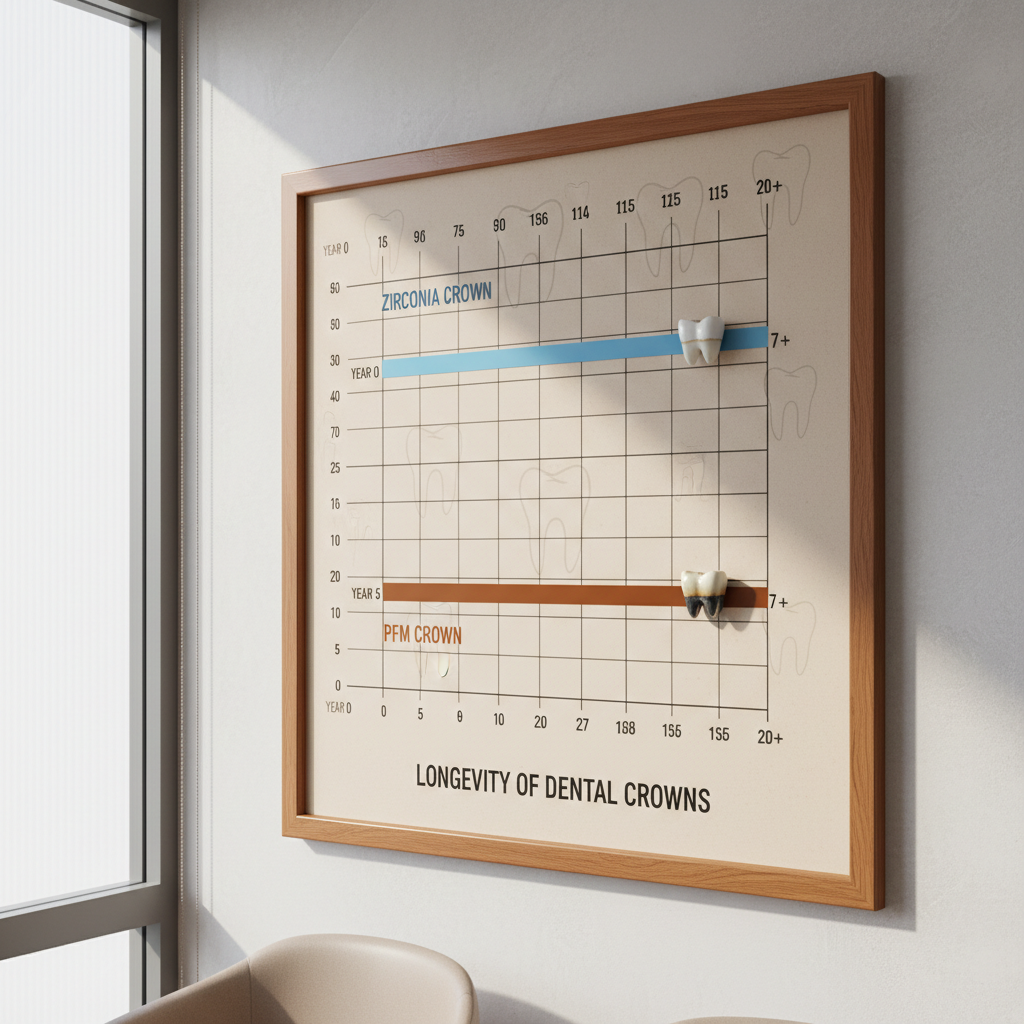
What Are The Durability Differences?

Durability remains a paramount concern for posterior restorations bearing heavy occlusal loads daily. This is where it gets interesting: monolithic zirconia has virtually eliminated a chipping problem known as “delamination.” Solid zirconia crowns withstand biting forces exceeding 1000 MPa, making them practically indestructible in typical mouth environments.
PFM units possess a strong metal core, but a weak link exists at any metal-ceramic interface. Cohesive failure regarding veneering porcelain occurs frequently under stress, leaving rough metal exposed to the tongue. While a framework rarely breaks, cosmetic failure requires replacement and creates patient dissatisfaction.
Recent studies show zirconia causes less wear on opposing dentition when polished correctly compared against abrasive feldspathic porcelain used on PFMs. Sourcing durable zircon sand derived materials ensures that milled crowns maintain their physical properties post-sintering. Strength without abrasiveness represents an ideal balance for long-term oral health maintenance.
| Characteristic | Monolithic Zirconia | PFM (Porcelain Fused to Metal) | |
|---|---|---|---|
| Chip Resistance | Extremely High | Moderate (Porcelain shears off) | |
| Fracture Strength | > 900 MPa | Metal is strong, Porcelain is weak | |
| Occlusal Wear | Low (if polished) | High (Porcelain is abrasive) | |
| Long-Term Integrity | Excellent | Good, but aesthetics fade |
How Biocompatible Are These Materials?
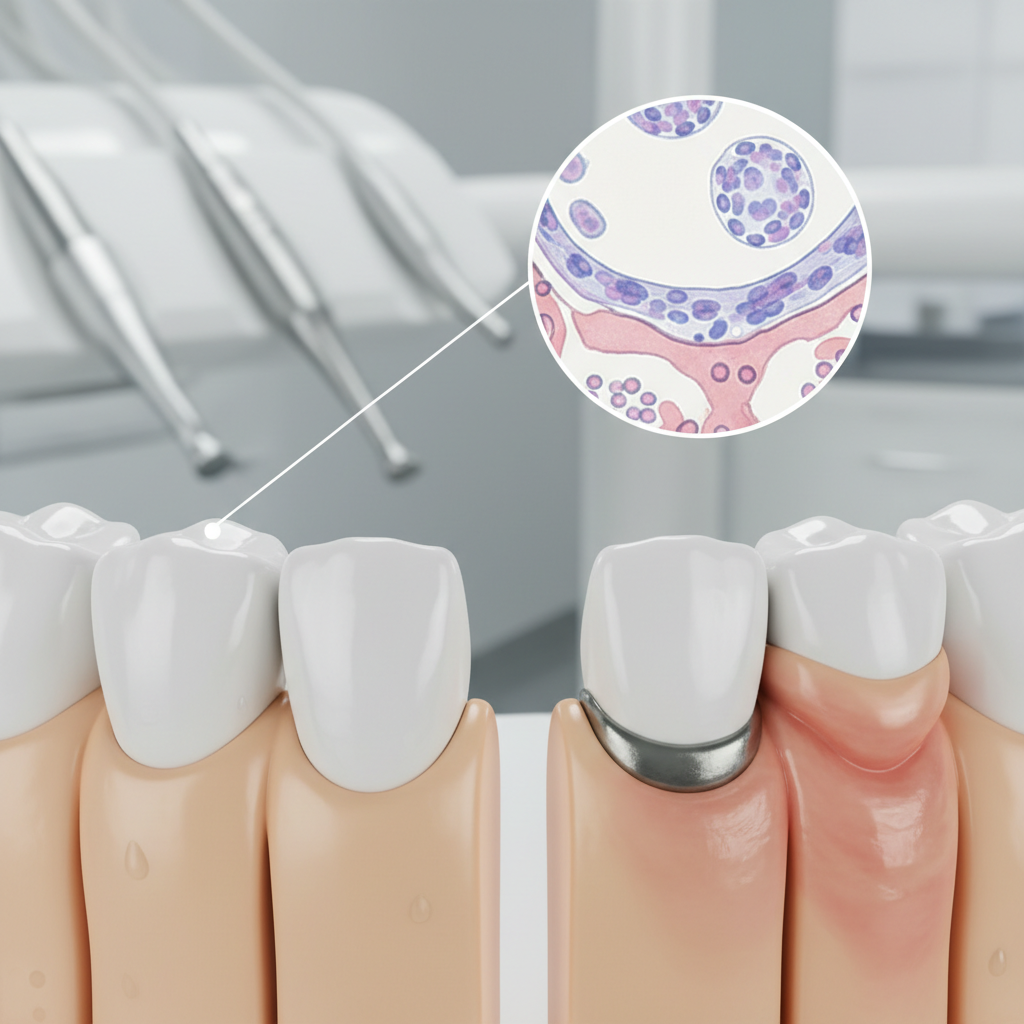
Biological integration determines longevity for any medical device implanted in a human body. Why does this matter? Zirconia classifies as a bio-inert material, meaning it triggers no adverse reaction from surrounding gingival tissues. Gingival cells adhere well onto polished zirconia surfaces, promoting a healthy seal against bacteria invasion.
PFM crowns pose risks for patients having metal sensitivities or allergies. Nickel and beryllium, common in base metal alloys, frequently cause allergic contact dermatitis or gingival inflammation known as “amalgam tattoo” sometimes. Even noble metals can conduct temperature, causing sensitivity for patients with vital pulps remaining.
Zirconia’s smooth surface inhibits plaque retention better than standard porcelain or metal margins. This characteristic reduces periodontal disease risks around restoration margins significantly. For dental labs, marketing biocompatible solutions utilizing high-grade zircon powder helps attract dentists focused on holistic and patient-safe practices.
| Property | Zirconia | PFM | |
|---|---|---|---|
| Allergy Risk | Extremely Low | Moderate (Nickel/Cobalt) | |
| Gingival Response | Healthy, Pink | Potential Inflammation/Graying | |
| Thermal Sensitivity | Insulating | Conductive | |
| Corrosion | None | Potential in mouth environment | |
| Plaque Affinity | Low | Moderate |
What Is The Manufacturing Process?

Manufacturing methods have revolutionized dental lab operations through automation and digitization. Ready for the good part? Zirconia production relies almost exclusively on digital workflows using advanced scanners. Technicians scan impressions, design restorations virtually (CAD), and mill them from pre-sintered discs (CAM) with micron-level precision. This process removes manual waxing, investing, and casting variables that cause errors.
PFM fabrication involves a labor-intensive “lost-wax” technique requiring skilled hands. Creating metal copings requires multiple manual steps, each introducing potential error and fit discrepancies. Porcelain layering also demands high artistic skill and time, creating bottlenecks in production flow during busy periods.
Digital manufacturing utilizing quality products enables labs to scale output without sacrificing precision or quality. Automated milling machines run overnight, drastically reducing turnaround times for urgent cases. This efficiency gain allows competitive pricing while maintaining healthy profit margins for dental businesses facing competition.
How Do Costs Compare For Businesses?
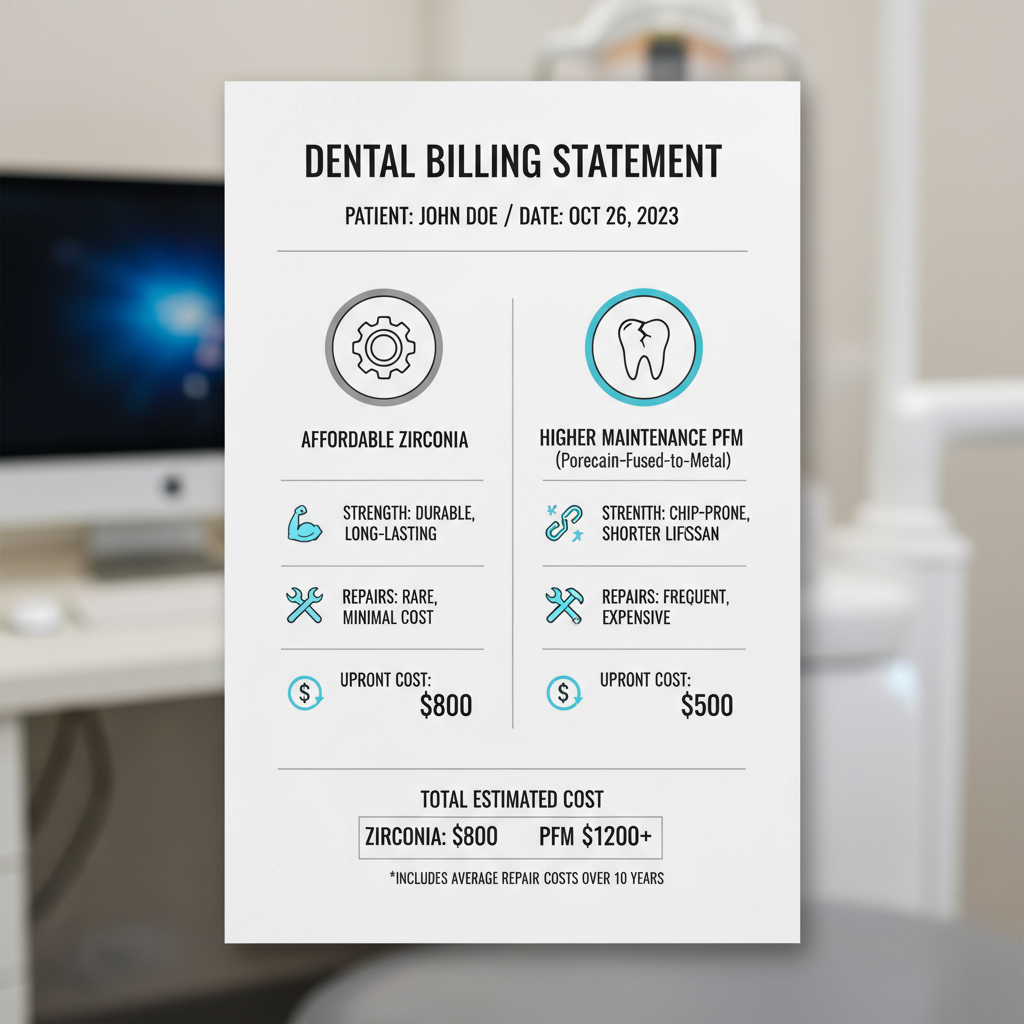
Financial viability drives business decisions for labs and clinics alike. Here’s the bottom line: while raw zirconia discs may cost more than some base metal alloys, massive reduction in labor hours changes an equation. A monolithic zirconia crown requires significantly less bench time than a PFM unit does.
PFM production incurs hidden costs through alloy fluctuations (especially gold prices) and skilled labor requirements. Finding experienced ceramists becomes increasingly difficult and expensive in today’s labor market. Conversely, digital technicians can manage high volumes regarding zirconia designs efficiently with less physical fatigue.
Investment in milling equipment pays off through volume and consistency gains. Reducing remake rates by using reliable zirconium materials further protects profitability over fiscal quarters. Ultimately, zirconia offers a more predictable cost structure for modern dental laboratories planning growth.
What Are The Clinical Indications?
Dentists need clear guidelines for material selection to ensure clinical success. It turns out, zirconia serves a wider range of indications today than ever before. High-strength zirconia suits long-span bridges and bruxer cases where PFM might fracture under load. Its ability to be milled thin allows for conservative tooth preparation, preserving precious enamel.
PFM still holds value for complex attachments or cases requiring precision metal rests for partial dentures. However, these specific scenarios become rarer as digital dentistry evolves toward implants. For standard single crowns and 3-unit bridges, zirconia has become a default standard of care globally.
Clinicians appreciate versatility regarding cementing or bonding zirconia restorations. Modern primers enhance adhesion, making retention reliable even with short preparations or tapered walls. Offering a comprehensive range of zirconia options positions a lab as a versatile partner for any clinical need arising.
| Indication | Zirconia Suitability | PFM Suitability | |
|---|---|---|---|
| Single Posterior | Excellent (Monolithic) | Good | |
| Single Anterior | Excellent (Layered/HT) | Good (Opaque Core risk) | |
| Long-Span Bridge | Good (High Strength) | Good (Metal framework) | |
| Bruxism Patient | Excellent | Poor (Porcelain chips) | |
| Limited Space | Excellent (Thin milling) | Fair (Requires bulk) |
How Should Dental Labs Choose?

Selecting a material partner defines a lab’s product quality and reputation. Let’s be honest: not all zirconia discs offer equal performance or aesthetic results. Variations in binder distribution or chemical purity lead toward warping during sintering cycles. Labs must verify that their supplier adheres strictly to ISO standards.
We prioritize consistency in our manufacturing processes for every batch produced. This ensures that every batch behaves identically in a mill and furnace setup. Reliable shrinkage factors mean fitting crowns immediately without hours spent on manual adjustment or re-milling.
Support from a manufacturer matters for troubleshooting issues. Technical guidance on sintering curves and bur strategies helps labs optimize their equipment usage. Partnering with a dedicated industrial supplier secures a stable supply chain, protecting your business from market volatility and shortages.
What Does The Future Hold?
Dental technology never stands still for long. You might be surprised, but future trends point toward even more advanced ceramics dominating the market. Multi-layer discs with built-in color and strength gradients already reduce needs for external staining significantly. This evolution continues pushing PFM further into obsolescence for standard procedures.
Research into zirconia-based resins for 3D printing holds massive promise for efficiency. While milling dominates today, additive manufacturing could reduce material waste significantly in coming years. Staying ahead requires aligning with manufacturers who invest heavily in R&D and innovation cycles.
As an industry moves toward total digitization, reliance on consistent, high-quality zirconium materials will only grow stronger. Positioning your business at a forefront regarding this ceramic revolution ensures long-term relevance and success in a competitive market.
| Trend | Impact on Labs | Impact on Clinicians | |
|---|---|---|---|
| Multi-Layer Blanks | Reduced staining labor | Better aesthetics | |
| Faster Sintering | Same-day production | Quick turnaround | |
| 3D Printed Ceramics | Less material waste | Lower costs eventually | |
| AI Design | High volume capacity | Consistent morphology |
Conclusion
Zirconia clearly surpasses PFM in durability, aesthetics, and manufacturing efficiency for most modern dental applications. To sum up, transitioning to high-quality zirconia workflows empowers labs to deliver superior results while optimizing operational costs effectively. We invite you to explore our premium Zirconia solutions to elevate your production standards today.
FAQ
Q1: What distinguishes zirconia from PFM regarding strength?Zirconia offers superior flexural strength, often exceeding 1000 MPa, whereas PFM relies on a metal core that can suffer from porcelain veneer chipping under pressure.
Q2: Does zirconia cost more than PFM for laboratories?While equipment costs exist, reduced labor hours and material consistency often make zirconia more cost-effective per unit than labor-intensive PFM fabrication.
Q3: Can zirconia match the aesthetics of natural teeth?Yes, modern high-translucency zirconia and multi-layer discs provide gradients and light transmission that closely mimic natural dentition layers.
Q4: Is zirconia considered safe for patients with allergies?Zirconia remains a metal-free, bio-inert material, making it an excellent choice for patients having sensitivities to metals like nickel or cobalt.
Q5: How does the manufacturing process differ?Zirconia utilizes efficient digital CAD/CAM milling workflows, while PFM requires manual waxing, casting, and porcelain layering steps that take longer.