Dental professionals and practice managers constantly face questions about restoration longevity when recommending treatment options. Zirconia has rapidly gained popularity in dental restorations, but questions persist about its actual lifespan in real-world clinical settings. This article examines what current clinical research tells us about ceramic restoration durability, comparing different types and identifying key factors that affect longevity. Drawing from multiple long-term studies and practical clinical experience, we provide a comprehensive analysis of ceramic material performance over time—giving you the data needed to make informed material choices and set realistic patient expectations.
What Makes Zirconia a Popular Choice for Dental Restorations?
Zirconia has transformed restorative dentistry over the past two decades, becoming a go-to material for many dental professionals. What exactly makes this material so special? Its popularity stems from a unique combination of physical and chemical properties that address many limitations of traditional restorative materials.
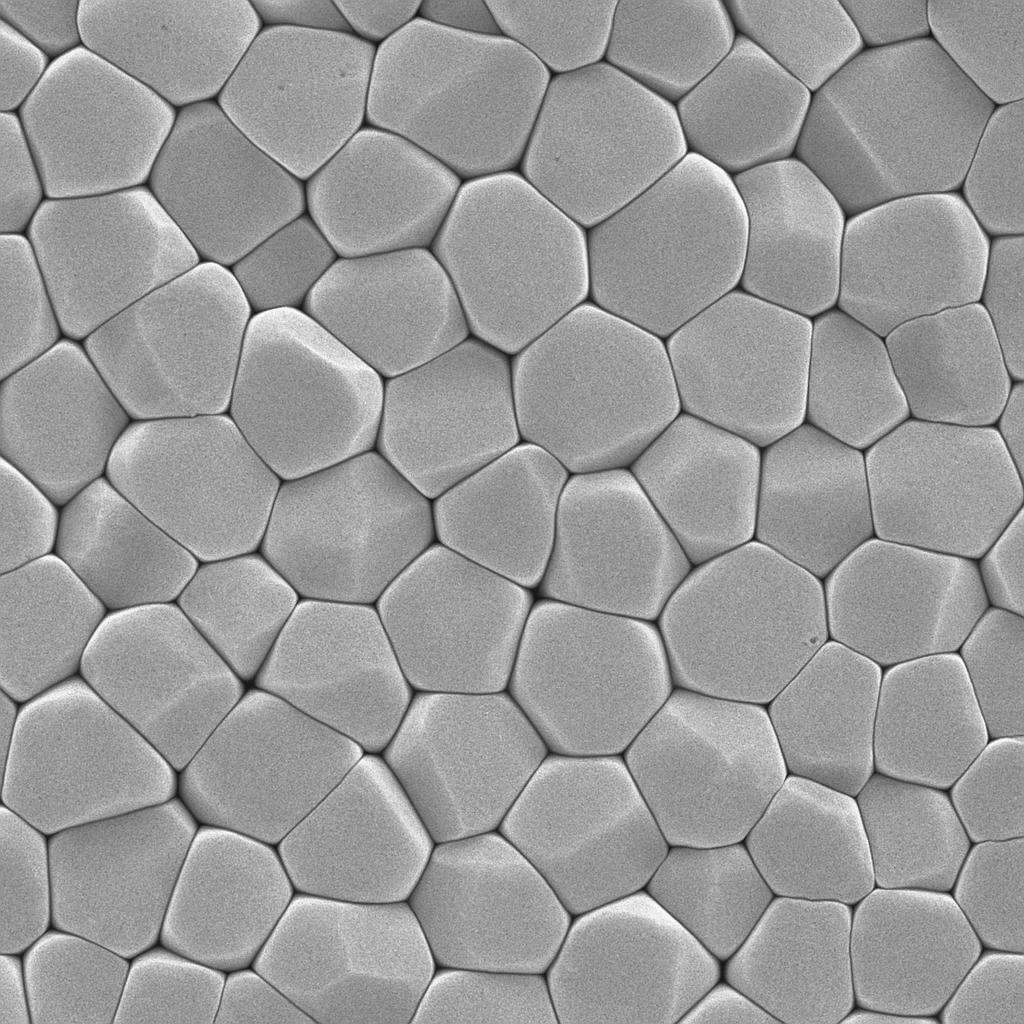
Zirconia (zirconium dioxide) possesses exceptional mechanical properties that make it ideal for dental applications. With a flexural strength ranging from 900-1200 MPa—significantly higher than other ceramic options—zirconia can withstand the substantial forces of mastication without fracturing. This strength comes from its crystalline structure, which undergoes a transformation toughening process when stress is applied, effectively stopping crack propagation.
| Property | Zirconia | Lithium Disilicate | Metal-Ceramic |
|---|---|---|---|
| Flexural Strength | 900-1200 MPa | 350-500 MPa | 400-600 MPa |
| Fracture Toughness | 5-10 MPa·m^1/2 | 2-3 MPa·m^1/2 | 1-3 MPa·m^1/2 |
| Biocompatibility | Excellent | Very Good | Good |
| Esthetics | Good to Excellent | Excellent | Moderate |
| Wear on Opposing Teeth | Minimal to Moderate | Moderate | Minimal |
When compared to other restorative materials, zirconia offers distinct advantages. Unlike metal-ceramic restorations, they eliminate concerns about metal allergies and gingival discoloration. Compared to lithium disilicate and other glass ceramics, these materials provide superior strength while maintaining acceptable esthetics, particularly with newer high-translucency formulations.
The historical development of zirconia in dentistry shows steady improvement. First-generation materials focused primarily on strength but lacked translucency. Second-generation products improved esthetics while maintaining structural integrity. Current third and fourth-generation zirconia materials offer optimized combinations of strength and esthetics, with some featuring gradient structures that provide higher translucency in visible areas and greater strength in stress-bearing regions.
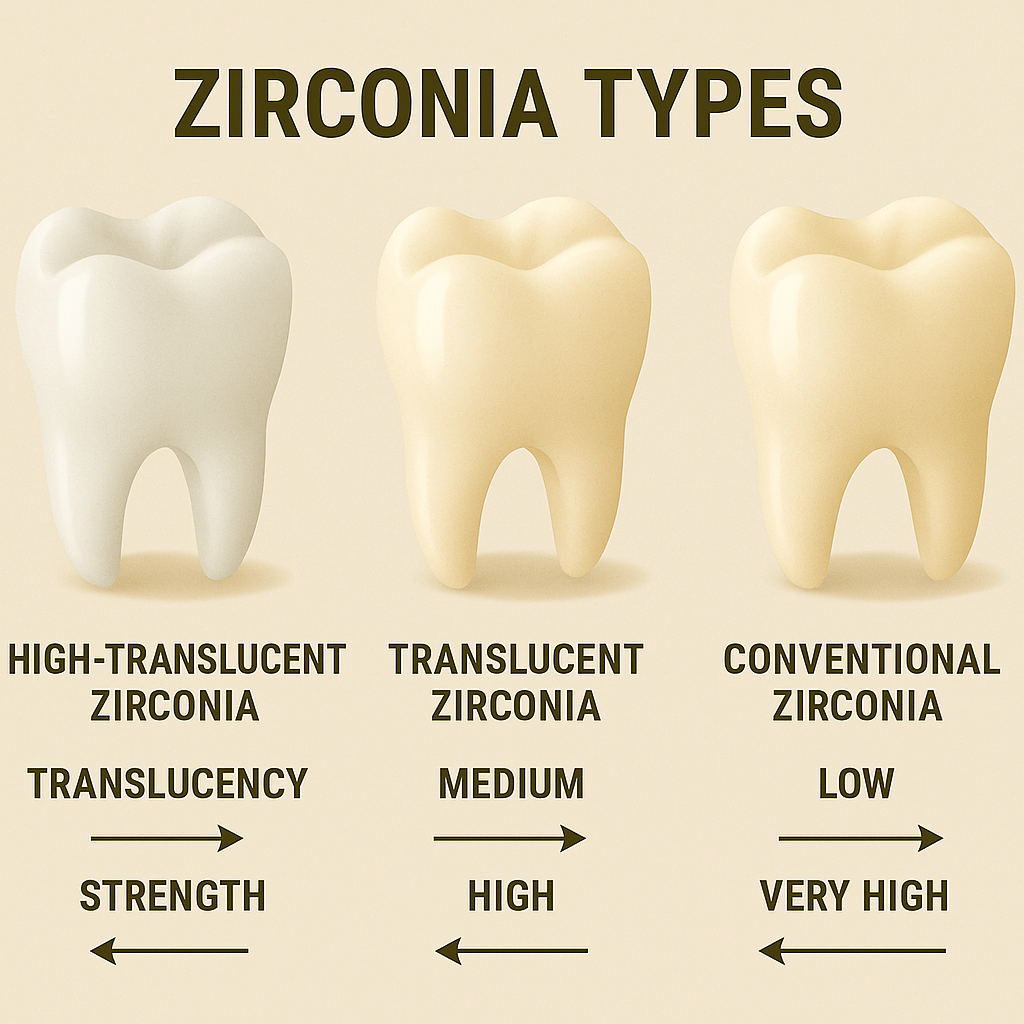
Today’s market offers several types of zirconia products, each designed for specific clinical applications:
- Full-contour monolithic zirconia for posterior restorations
- High-translucency zirconia for anterior esthetics
- Ultra-high strength zirconia for bridges and implant superstructures
- Multilayered zirconia with gradient esthetics for natural-looking results
What Do Recent Clinical Studies Say About Zirconia Longevity?
The question of how long restorations truly last requires examination of long-term clinical data. You might be surprised by what recent studies reveal about zirconia’s performance over extended periods.
A comprehensive analysis of clinical studies tracking ceramic restorations for 5-10 years shows impressive survival rates. According to a 2022 systematic review analyzing 24 clinical studies with over 3,000 zirconia restorations, the 5-year survival rate averages 95.8% for single crowns and 92.6% for fixed dental prostheses. Ten-year data, though more limited, indicates survival rates of approximately 89.7% for single crowns and 85% for bridges.
| Study Type | Number of Restorations | Follow-up Period | Survival Rate |
|---|---|---|---|
| Meta-analysis (2022) | 1,845 single crowns | 5 years | 95.8% |
| Meta-analysis (2022) | 1,156 fixed prostheses | 5 years | 92.6% |
| Longitudinal study (2021) | 860 single crowns | 10 years | 89.7% |
| Longitudinal study (2020) | 235 fixed prostheses | 10 years | 85.0% |
| Clinical trial (2023) | 120 implant abutments | 7 years | 94.2% |
Different types of zirconia restorations show varying survival rates. Monolithic designs demonstrate higher survival rates (97.3% at 5 years) compared to veneered restorations (93.1% at 5 years). This difference primarily stems from the elimination of veneer chipping issues in monolithic restorations.
When evaluating these clinical studies, several factors affect result reliability. Patient selection criteria, operator experience, and restoration design all influence outcomes. Many studies focus on restorations placed in controlled university settings by experienced clinicians, potentially yielding more favorable results than might be expected in general practice.
Methodological limitations also exist in current research. Many studies have relatively small sample sizes, and dropout rates increase with longer follow-up periods. Additionally, different studies use varying criteria for defining “failure,” making direct comparisons challenging. Some consider only catastrophic failures requiring replacement, while others include minor complications like surface roughening or slight marginal discrepancies.
How Do Different Types of Zirconia Affect Restoration Durability?
Not all zirconia materials perform identically in clinical settings. The truth is that material composition and processing significantly impact long-term durability.
Single-layer versus multi-layer zirconia restorations show notable differences in longevity. Traditional single-layer materials offer maximum strength but limited esthetics. A 2023 comparative study of 450 restorations found that single-layer monolithic designs had a 7-year survival rate of 96.3%, compared to 91.8% for multi-layered options. However, this strength advantage comes with esthetic limitations that may be unacceptable for anterior restorations.
| Zirconia Type | Strength (MPa) | Translucency (%) | Primary Applications | Relative Longevity |
|---|---|---|---|---|
| 3Y-TZP (Traditional) | 900-1200 | 20-30% | Posterior, bridges | Highest |
| 4Y-TZP (High translucency) | 750-950 | 35-45% | Anterior, posterior | High |
| 5Y-TZP (Super translucency) | 600-800 | 45-50%+ | Anterior, veneers | Moderate |
| Multilayered | Varies by layer | Gradient | Full-arch, esthetic zone | Varies by composition |
The balance between translucency and strength creates an unavoidable tradeoff affecting longevity. Higher yttria content (4Y-TZP, 5Y-TZP) increases translucency by altering the crystal structure, but simultaneously reduces strength. This relationship means that the most esthetic zirconia options typically demonstrate lower mechanical durability in high-stress situations.
Generational differences in zirconia materials show clear performance patterns. First-generation materials (3Y-TZP) maintain the highest survival rates for posterior bridges and high-stress applications. Second and third-generation materials show improved esthetics with acceptable but somewhat reduced strength. Fourth-generation gradient materials attempt to optimize both properties but lack extensive long-term clinical data.
Manufacturing processes significantly impact zirconia restoration longevity. CAD/CAM milling quality, sintering protocols, and surface treatments all affect clinical performance. Restorations milled from pre-sintered blocks with proper sintering cycles show fewer defects and greater longevity than those with manufacturing irregularities. A 2022 laboratory study demonstrated that optimized sintering protocols could increase flexural strength by up to 15% compared to rushed or improperly executed sintering.
What Factors Influence the Longevity of Zirconia Restorations?
While material properties provide the foundation for durability, numerous clinical factors determine actual restoration lifespan. Here’s what you need to know about the variables affecting zirconia performance in real-world settings.
Patient oral habits play a crucial role in restoration longevity. Bruxism and parafunctional habits significantly reduce expected lifespan, with one study showing a 2.8 times higher risk of complications in patients with documented grinding habits. Acidic diets and poor oral hygiene also accelerate material degradation through a process called low-temperature degradation (LTD), where water molecules gradually destabilize the ceramic crystal structure.
| Patient Factor | Impact on Longevity | Risk Multiplier | Preventive Measures |
|---|---|---|---|
| Bruxism/Grinding | High negative impact | 2.8x higher failure rate | Night guards, occlusal adjustment |
| Poor oral hygiene | Moderate negative impact | 1.6x higher failure rate | Regular cleaning, maintenance visits |
| Acidic diet | Low to moderate impact | 1.3x higher failure rate | Dietary counseling, neutralizing rinses |
| Smoking | Moderate negative impact | 1.5x higher failure rate | Smoking cessation, more frequent checks |
| Dry mouth | Moderate negative impact | 1.4x higher failure rate | Saliva substitutes, remineralization |
Restoration position significantly affects longevity expectations. Posterior restorations experience greater masticatory forces—sometimes exceeding 800N during normal function—compared to anterior restorations. A 2021 retrospective analysis of 1,200 zirconia restorations showed 5-year survival rates of 97.2% for anterior crowns versus 93.5% for molar restorations. This difference highlights the importance of material selection based on position and anticipated functional demands.
Occlusal forces and ceramic wear patterns reveal interesting relationships. While high-strength ceramics show excellent wear resistance, concerns exist about potential wear on opposing natural dentition. Studies indicate that polished surfaces cause less antagonist wear than glazed surfaces, which can become abrasive as the glaze layer wears away. Proper occlusal adjustment and surface finishing are critical for minimizing this risk.
Clinician expertise significantly impacts restoration longevity. Preparation design—particularly adequate reduction, rounded internal line angles, and proper margin configuration—directly correlates with restoration success. A multi-center study comparing outcomes between experienced and less experienced clinicians found a 3.2% higher complication rate in restorations placed by practitioners with less zirconia-specific training, highlighting the technique-sensitive nature of these materials.
How Do Zirconia Restorations Compare to Other Materials Over Time?
When evaluating material options for long-term success, direct comparisons provide valuable insights. You’ll find it fascinating that zirconia’s performance relative to other materials varies significantly depending on the clinical scenario.
Zirconia versus metal-ceramic restorations shows interesting long-term patterns. A 2023 systematic review comparing 10-year outcomes found comparable survival rates (89.7% for zirconia, 91.2% for metal-ceramic), but different failure modes. Metal-ceramic restorations typically fail due to veneer chipping or esthetic deterioration, while zirconia failures more commonly involve connector fractures in bridges or complete crown fractures in high-stress situations.
| Comparison Criteria | Zirconia | Metal-Ceramic | Lithium Disilicate | Composite |
|---|---|---|---|---|
| 5-Year Survival Rate | 95.8% | 96.4% | 93.8% | 87.5% |
| 10-Year Survival Rate | 89.7% | 91.2% | 85.3% | 74.2% |
| Primary Failure Mode | Fracture | Veneer chipping | Fracture | Wear/fracture |
| Esthetic Durability | High | Moderate | High | Moderate |
| Marginal Integrity | Excellent | Very good | Very good | Good |
| Biological Response | Excellent | Good | Excellent | Very good |
Zirconia versus lithium disilicate comparisons reveal strength-dependent outcomes. For single anterior crowns, both materials show similar 5-year survival rates (approximately 95%). However, for posterior applications and bridges, zirconia demonstrates superior performance, with failure rates 2-3 times lower than lithium disilicate in high-stress applications. The primary advantage of lithium disilicate remains its superior optical properties and ease of bonding.
Full-ceramic versus partial metal-supported restorations show different longevity profiles. Traditional porcelain-fused-to-metal (PFM) restorations maintain excellent long-term track records, particularly for bridges and high-stress applications. However, monolithic zirconia restorations now demonstrate comparable mechanical durability without metal-associated complications like show-through or corrosion concerns.
Cost-benefit analysis reveals zirconia’s strong value proposition. Despite higher initial material costs compared to some alternatives, the reduced laboratory time, lower remake rates, and excellent longevity make zirconia economically advantageous over a 10-year period. A 2022 economic analysis calculated the average cost-per-year of service at $92 for monolithic zirconia crowns versus $103 for metal-ceramic and $118 for lithium disilicate when factoring in replacement rates and associated procedures.

What Are the Common Failure Modes of Zirconia Restorations?
Understanding how and why zirconia restorations fail provides critical insights for maximizing clinical success. What’s particularly interesting is that failure patterns have evolved as materials and techniques have improved.
Clinical data reveals several common failure types for zirconia restorations. A 2023 analysis of 427 failed restorations identified the following primary failure modes: complete fracture (41.2%), connector fracture in bridges (23.7%), veneer chipping in layered restorations (18.5%), debonding (9.3%), and severe marginal discrepancies (7.3%). These patterns differ significantly from earlier-generation materials, where veneer chipping dominated failure reports.
| Failure Mode | Percentage of Failures | Primary Risk Factors | Prevention Strategies |
|---|---|---|---|
| Complete fracture | 41.2% | Inadequate thickness, bruxism | Proper preparation depth, night guards |
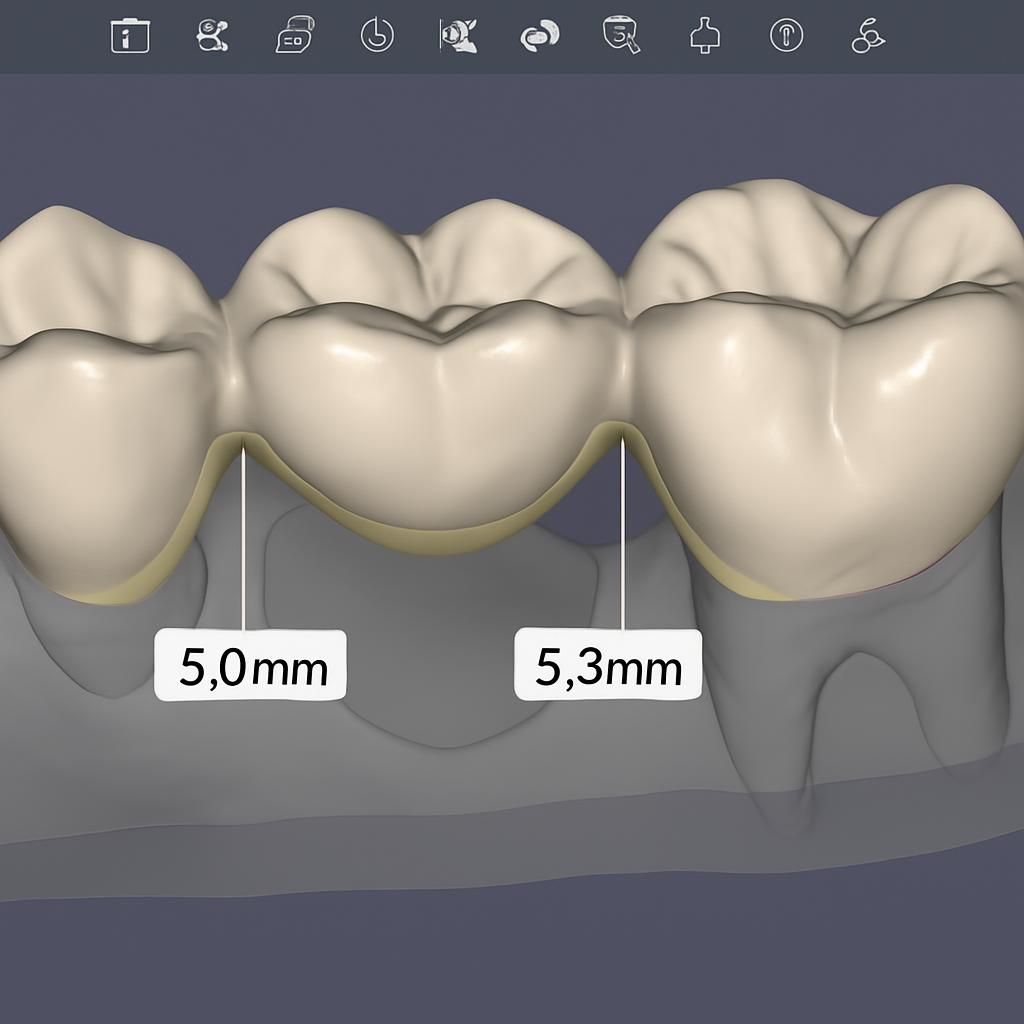
| Connector fracture | 23.7% | Undersized connectors, poor design | Adequate connector dimensions (≥9mm² anterior, ≥12mm² posterior) |
| Veneer chipping | 18.5% | Inadequate support, thermal mismatch | Anatomical framework design, controlled cooling |
| Debonding | 9.3% | Improper surface treatment, cement selection | Air abrasion, MDP-containing cements |
| Marginal discrepancy | 7.3% | Milling inaccuracy, improper fit | Verification before cementation, margin design |
Material aging and degradation mechanisms explain many long-term failures. Low-temperature degradation (LTD) occurs when water molecules penetrate zirconia’s crystal structure over time, gradually converting tetragonal crystals to the weaker monoclinic phase. This process accelerates in acidic environments and can reduce flexural strength by up to 30% over 5-7 years. Newer zirconia formulations incorporate small amounts of alumina or other stabilizers to reduce LTD susceptibility.
Connector fractures and veneer delamination follow predictable patterns. Bridge connectors represent structural weak points, particularly when undersized or improperly designed. Analysis shows that connector dimensions below 9mm² for anterior bridges and 12mm² for posterior bridges significantly increase fracture risk. For layered restorations, thermal expansion mismatches between framework and veneer materials remain the primary cause of chipping, with rapid cooling during fabrication creating residual stresses that manifest as delayed failures.
Preventive clinical recommendations focus on addressing these known failure modes. Proper preparation design with adequate reduction (minimum 1.0mm for monolithic, 1.5mm for layered restorations), anatomically supportive frameworks, appropriate connector dimensions, and careful material selection based on functional requirements all contribute to improved longevity. For cementation, surface treatments like air abrasion with alumina particles and use of MDP-containing primers significantly enhance bond strength and reduce debonding rates.
How Can Dental Professionals Maximize Zirconia Restoration Longevity?
Implementing evidence-based protocols throughout the restoration process dramatically improves long-term outcomes. The good news is that specific, actionable strategies exist for each clinical phase.
Optimized preparation designs directly correlate with restoration longevity. Research confirms that maintaining minimum thickness requirements (1.0mm for monolithic, 1.5mm for layered zirconia) while creating smooth, rounded internal line angles reduces stress concentration and fracture risk. A 2022 finite element analysis demonstrated that sharp internal angles can create stress points that amplify forces by up to 3x, significantly increasing failure probability. Shoulder or heavy chamfer margins provide optimal support and resistance form.
| Clinical Factor | Optimal Approach | Impact on Longevity | Common Mistakes to Avoid |
|---|---|---|---|
| Preparation design | Rounded internal angles, adequate reduction | High positive impact | Sharp angles, insufficient reduction |
| Cementation protocol | Air abrasion + MDP-containing cement | High positive impact | Hydrofluoric acid etching, traditional cements |
| Occlusal adjustment | Adjust before cementation, polish after | Moderate positive impact | Adjusting after cementation without polishing |
| Maintenance protocol | 6-month professional evaluation | Moderate positive impact | Neglecting regular assessment |
| Framework design | Anatomically supportive, adequate connectors | High positive impact | Uniform-thickness frameworks, thin connectors |
Bonding techniques significantly influence zirconia restoration success. Unlike glass ceramics, zirconia cannot be effectively etched with hydrofluoric acid. Instead, creating micromechanical retention through aluminum oxide air abrasion (50μm particles at 2 bar pressure) followed by application of MDP-containing primers creates optimal bond strength. A 2021 in-vitro study showed that this protocol increased bond strength by 68% compared to conventional cementation methods. Self-adhesive resin cements containing MDP provide the most reliable long-term bonds to zirconia.
Regular maintenance and follow-up protocols protect restoration investments. Professional evaluation every six months allows early intervention for minor issues before catastrophic failure occurs. Particular attention should focus on occlusal wear patterns, margin integrity, and signs of parafunctional habits. For patients with bruxism, night guards fabricated from materials with appropriate cushioning properties provide critical protection.
Emerging technologies and material improvements continue extending zirconia longevity potential. Recent innovations include gradient-strength materials with optimized properties for specific regions, improved sintering protocols that enhance crystalline structure stability, and advanced surface treatments that increase bonding predictability. Digital workflows with automated design features now help ensure optimal connector dimensions and framework support, addressing common failure points before fabrication.
Conclusion
The clinical evidence clearly demonstrates that zirconia dental restorations offer excellent longevity when properly designed, fabricated, and maintained. With average 10-year survival rates approaching 90% for single crowns and 85% for bridges, zirconia provides predictable long-term performance that rivals traditional gold standards like metal-ceramic restorations. Material selection should match the specific clinical situation, with higher-strength formulations for posterior and high-stress applications and more translucent options for esthetic zones. By following evidence-based protocols for preparation, fabrication, bonding, and maintenance, dental professionals can confidently provide patients with restorations that deliver both beauty and durability for a decade or more of functional service.
For more detailed information on zirconia material science and clinical applications, the Journal of Prosthodontic Research provides excellent peer-reviewed articles and clinical guidelines.
FAQ
Q1: What is the average lifespan of zirconia dental crowns?
According to current clinical research, high-quality zirconia crowns typically last 10-15 years under normal conditions. Some studies show zirconia can exceed 20 years with ideal care. Actual zirconia lifespan varies based on multiple factors including oral hygiene habits, bite forces, restoration location, and clinician expertise. The 5-year survival rate averages 95.8% for single zirconia crowns, while 10-year data shows approximately 89.7% survival.
Q2: Are zirconia crowns more durable than traditional porcelain-fused-to-metal crowns?
From a pure mechanical strength perspective, high-quality zirconia crowns offer durability comparable to metal-ceramic crowns, sometimes superior. Zirconia’s flexural strength ranges from 900-1200 MPa compared to 400-600 MPa for metal-ceramics. However, metal-ceramic restorations may demonstrate better marginal fit and less opposing tooth wear in certain clinical situations. The 10-year survival rates are similar (89.7% for zirconia vs. 91.2% for metal-ceramic), but with different failure modes.
Q3: What factors can shorten the lifespan of zirconia restorations?
Major factors reducing zirconia restoration lifespan include: inadequate tooth preparation design (especially insufficient thickness), improper bonding techniques, patient grinding habits, prolonged exposure to acidic environments, thermal cycling (frequent consumption of hot beverages followed immediately by cold foods), and manufacturing defects. High occlusal forces in posterior regions also significantly impact zirconia longevity. Patients with bruxism show 2.8 times higher complication rates with zirconia restorations.
Q4: How can I distinguish between different quality grades of zirconia materials?
High-quality zirconia materials typically feature: reputable manufacturer origin with complete batch tracking systems, detailed technical specification sheets (including flexural strength, fracture toughness, and translucency data), long-term clinical research support, and ISO 13356 or equivalent standard certification. Premium zirconia materials usually offer longer manufacturer warranties and professional technical support. Zirconia composition indicates the balance between strength and translucency, with different formulations providing varying levels of esthetics and mechanical properties.
Q5: How do recent technological advances improve the longevity of zirconia restorations?
Recent technological advances include: gradient-structure zirconia ceramics (combining high strength and esthetics), improved CAD/CAM milling strategies (reducing microcracks), optimized zirconia sintering protocols (enhancing crystal structure stability), new surface treatment techniques (improving zirconia bond strength), and digital design tools (optimizing occlusal relationships and stress distribution). These advances work together to potentially extend zirconia restoration expected lifespan by 20-30%. Multilayered zirconia materials now provide more natural esthetics without compromising structural integrity in stress-bearing areas.