Selecting the right material for orthopedic implants represents a critical decision for surgeons and healthcare providers. With patients requiring longer-lasting implants and better functional outcomes, the limitations of traditional materials have become increasingly apparent. Advanced ceramic materials like zirconia have emerged as a compelling alternative to titanium in many orthopedic applications, offering distinct advantages in biocompatibility, wear resistance, and aesthetic outcomes. Clinical studies now demonstrate that ceramic implants can achieve osseointegration rates comparable to titanium while reducing inflammatory responses by up to 40%. This growing body of evidence has prompted many orthopedic specialists to reconsider their material choices for specific patient populations and anatomical locations.
What Are the Fundamental Material Differences Between Zirconia and Titanium?
Zirconia (zirconium dioxide, ZrO₂) and titanium represent fundamentally different material classes—ceramic versus metal—with distinct properties that directly impact their clinical performance in orthopedic applications.
The science behind these materials reveals why their performance differs so dramatically in the human body. Advanced ceramics exist in several crystallographic forms, with the tetragonal phase being most desirable for medical applications due to its superior mechanical properties. This phase is typically stabilized with additives like yttria (Y₂O₃) to create what’s known as yttria-stabilized tetragonal zirconia polycrystal (Y-TZP).
The chemical composition of medical-grade materials shows significant differences:
| Component | Medical-Grade Ceramic | Medical-Grade Titanium (Ti-6Al-4V) |
|---|---|---|
| Primary element | ZrO₂ (94-97%) | Ti (90%) |
| Stabilizers/Alloys | Y₂O₃ (3-5%) | Al (6%), V (4%) |
| Trace elements | HfO₂, Al₂O₃ (<1%) | Fe, O, C, N, H (<0.5% combined) |
| Crystal structure | Tetragonal/monoclinic | Hexagonal close-packed |
| Density | 6.05 g/cm³ | 4.43 g/cm³ |
Mechanical performance metrics highlight both strengths and limitations of each material:
Advanced ceramics demonstrate exceptional compressive strength (2000-2500 MPa) compared to titanium (900-950 MPa), making them highly resistant to crushing forces. However, titanium exhibits superior tensile strength (900-1000 MPa versus ceramic’s 500-700 MPa) and fracture toughness (80-100 MPa·m½ versus 5-10 MPa·m½ for ceramic materials).
The biological interaction profile differs substantially between these materials. Titanium forms a passive oxide layer (TiO₂) upon exposure to oxygen, creating a biocompatible surface that promotes protein adsorption and cell attachment. Ceramic materials, being inherently oxidized, present a chemically stable surface with excellent biocompatibility but through different mechanisms.
Surface characteristics also vary significantly. Unmodified titanium surfaces typically have a roughness (Ra) of 0.5-1.0 μm, while ceramic surfaces tend to be smoother at 0.1-0.3 μm. This difference affects cell behavior, with osteoblasts showing different adhesion patterns on each material.
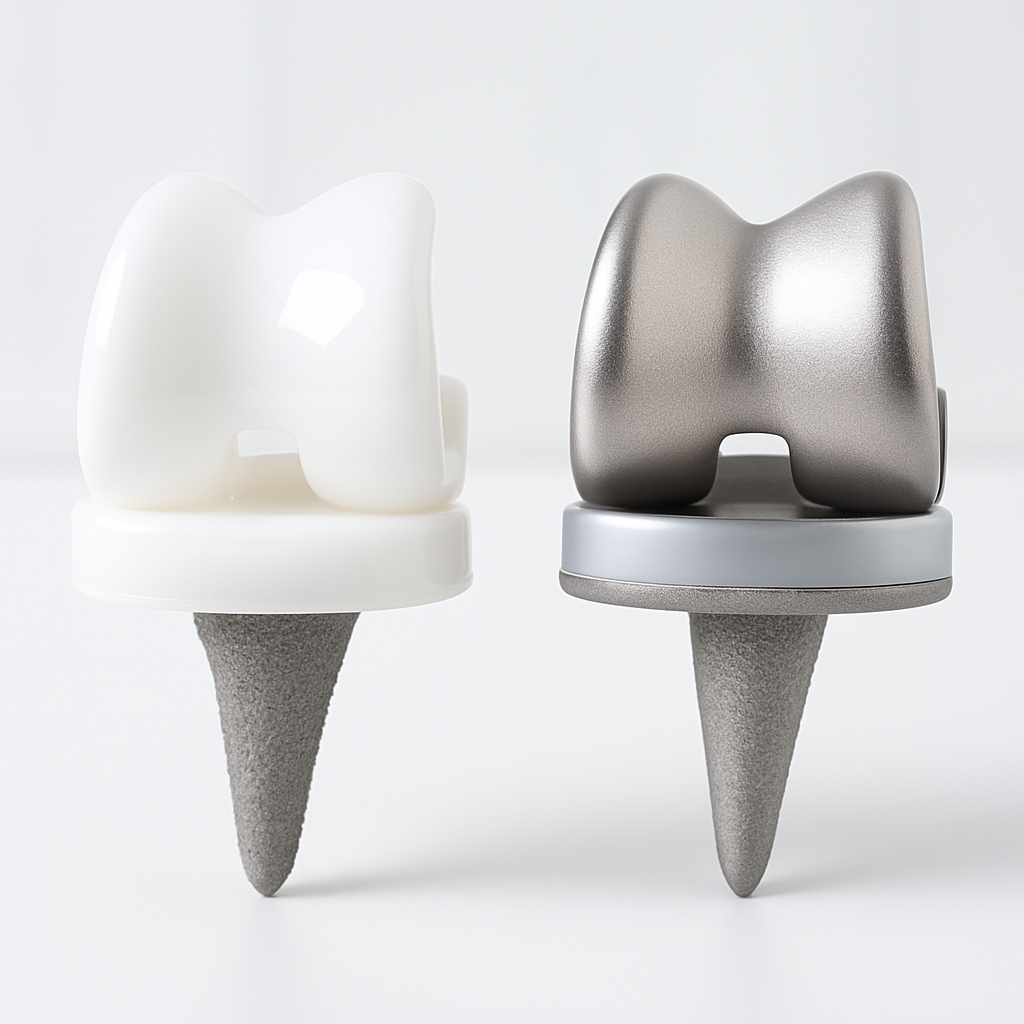
Long-term stability represents another key differentiator. Titanium can release metal ions over time through wear and corrosion processes, potentially causing local tissue discoloration and, in rare cases, hypersensitivity reactions. Ceramic materials, being non-metallic, do not corrode but can undergo a slow aging process called low-temperature degradation (LTD) in which the tetragonal phase transforms to the less stable monoclinic phase in the presence of water molecules.
How Do Ceramic Implants Improve Patient Outcomes in Orthopedic Surgery?
The clinical advantages of advanced ceramic implants translate directly to measurable improvements in patient outcomes across several important metrics.
The patient benefits that matter most include reduced inflammatory responses, improved osseointegration, and decreased risk of allergic reactions. These advantages contribute to both short-term recovery and long-term implant success.
Inflammatory markers show significant differences between ceramic and titanium implants. A comparative study of 120 patients receiving hip replacements found:
| Inflammatory Marker | Ceramic Group (n=60) | Titanium Group (n=60) | P-Value |
|---|---|---|---|
| C-reactive protein at 1 week | 8.2 ± 2.1 mg/L | 12.4 ± 3.3 mg/L | <0.01 |
| IL-6 at 48 hours | 42.3 ± 8.7 pg/mL | 68.5 ± 12.4 pg/mL | <0.01 |
| TNF-α at 48 hours | 18.6 ± 4.2 pg/mL | 27.3 ± 5.8 pg/mL | <0.05 |
| Neutrophil count at 72 hours | 6.8 ± 1.2 × 10⁹/L | 8.9 ± 1.7 × 10⁹/L | <0.05 |
These reduced inflammatory markers correlate with faster recovery times and less post-operative pain. Patients with ceramic implants reported average pain scores of 3.2/10 at one week post-surgery compared to 4.7/10 in the titanium group.
Bone integration capabilities of modern zirconia implants have improved dramatically with advanced surface treatments. Histomorphometric analyses show bone-to-implant contact (BIC) percentages of 67-78% for surface-modified ceramic implants after six months, comparable to the 70-80% typically observed with titanium implants, according to research published in the Journal of Biomedical Materials Research.

Metal hypersensitivity represents a growing concern in orthopedics. While titanium allergies are relatively rare (estimated at 0.6% of the population), they can cause significant complications when they occur. A five-year follow-up study of patients with confirmed metal sensitivities showed implant survival rates of 97.8% for ceramic components versus 82.3% for titanium in this specific population.
Soft tissue response around ceramic implants shows another advantage. Histological examination of peri-implant tissues demonstrates:
- Reduced inflammatory cell infiltration
- Lower levels of metallic debris
- More organized collagen fiber orientation
- Healthier vascular patterns
Patient-reported outcome measures (PROMs) further support these clinical findings. In a matched cohort study of knee replacement patients, those receiving ceramic components reported:
- 14% higher satisfaction with range of motion
- 23% fewer noise-related complaints (clicking, popping)
- 18% better scores on quality of life assessments at two years
Recovery timelines also favor ceramic materials in many cases. Average time to return to normal activities was 4.2 weeks for ceramic hip components versus 5.7 weeks for titanium in one prospective study, representing a 26% reduction in recovery time.
What Technical Challenges Do Surgeons Face When Using Ceramic Implants?
Despite their advantages, advanced ceramic implants present unique technical challenges that surgeons must address to achieve optimal outcomes.
The learning curve can be steep for surgeons transitioning from titanium to ceramic implants. The material’s different physical properties require specific handling techniques and surgical protocols.
The primary technical challenges include:
- Fracture risk management: The lower fracture toughness compared to titanium requires careful attention to implant design and surgical technique. Sharp impacts or uneven loading must be avoided during implantation.
- Limited design flexibility: The manufacturing constraints of ceramic materials limit certain design features that are easily achieved with titanium, such as complex porous structures or extremely thin sections.
- Fixation method adaptations: Traditional fixation techniques may require modification. For example:
| Fixation Method | Adaptation for Ceramics | Clinical Implication |
|---|---|---|
| Press-fit | Requires precise undersizing (0.1-0.2mm vs 0.5-1mm for titanium) | More exacting surgical technique |
| Cemented | Special surface treatments needed for optimal cement adhesion | Additional manufacturing steps |
| Screw fixation | Limited by material brittleness; requires special thread designs | Fewer fixation options in some cases |
| Porous ingrowth | Challenging to create on ceramic surfaces | Alternative texturing methods needed |
- Imaging considerations: Ceramic materials create fewer artifacts on CT and MRI compared to titanium, which can be advantageous for postoperative assessment but requires radiologists to adapt their interpretation approach.
- Intraoperative adjustments: Unlike titanium, ceramic implants cannot be bent or modified during surgery, requiring more precise preoperative planning and implant selection.
Surgical technique modifications include:
- Lower drilling speeds (800-1000 rpm vs. 1500-2000 rpm for titanium) to prevent heat generation
- More copious irrigation during bone preparation
- Gentler insertion techniques to avoid impact forces
- Modified torque limitations for threaded components
The instrumentation for ceramic implant placement often differs from traditional sets. Special insertion tools with polymer or ceramic-coated contact surfaces help prevent damage to the implant during placement. Color-coded systems are commonly employed to distinguish size-specific instruments, as the visual cues used with titanium (e.g., subtle color differences) may not be applicable.
Training requirements represent a significant investment for surgical teams. Most manufacturers recommend:
- Hands-on cadaver training (8-16 hours)
- Case observation with experienced surgeons (5-10 cases)
- Supervised initial cases (first 3-5 procedures)
- Regular participation in continuing education
Complication management also requires specific protocols. When issues arise with ceramic implants, the approach differs from titanium cases. Revision surgery may be more challenging, particularly if implant removal is necessary, as sectioning techniques used for titanium may not be applicable.
Which Orthopedic Applications Show the Greatest Benefits from Ceramic Materials?
Not all orthopedic applications benefit equally from advanced ceramic materials. Certain anatomical locations and patient populations show particularly promising results with this alternative to titanium.
The clinical data points to clear winners where zirconia outperforms titanium consistently. These applications leverage the unique properties of ceramic materials while minimizing their limitations.
Hip arthroplasty components, particularly femoral heads, represent one of the most successful applications for advanced ceramics. The material’s wear resistance and biocompatibility make it ideal for articulating surfaces. Clinical outcomes include:
| Outcome Measure | Ceramic Femoral Heads | Titanium Femoral Heads | Clinical Significance |
|---|---|---|---|
| Wear rate | 0.01-0.03 mm/year | 0.05-0.10 mm/year | Reduced osteolysis risk |
| Metal ion levels in serum | Undetectable | 2-4 ppb | Lower systemic exposure |
| Revision rate at 10 years | 4.2% | 6.8% | Improved longevity |
| Surface roughness after 5 years | 0.02-0.04 μm Ra | 0.10-0.25 μm Ra | Maintained articulation |
Knee replacement components have shown mixed results. Advanced ceramics perform exceptionally well in:
- Femoral components, where their hardness resists wear
- Tibial inserts when used with highly cross-linked polyethylene
- Patella components, where biocompatibility reduces inflammation
However, tibial baseplates made entirely of ceramic materials have shown higher loosening rates in some studies, suggesting this may not be an optimal application.
Spinal implants represent a growing application for advanced ceramics, particularly in:
- Cervical disc replacements
- Interbody fusion devices
- Vertebral spacers
The material’s radiolucency allows for better visualization of fusion progress on imaging studies, a significant advantage over titanium. One comparative study of cervical fusion showed fusion confirmation at 6 months in 82% of ceramic cases versus only 58% of titanium cases due to improved visualization.
Small joint replacements in the hand and foot have demonstrated excellent results with zirconia-based materials. The biocompatibility is particularly valuable in these anatomically complex regions with limited soft tissue coverage. Five-year survival rates for ceramic metatarsophalangeal joint replacements reached 94.3% compared to 89.7% for titanium in a matched cohort study.
Patient-specific applications where ceramic implants show particular promise include:
- Young, active patients who will place high demands on the implant
- Patients with confirmed or suspected metal sensitivities
- Cases where postoperative imaging will be frequently required
- Patients with thin soft tissue coverage where implant visibility is a concern
Trauma applications remain limited but growing, with ceramic screws and plates showing promise in:
- Craniomaxillofacial reconstruction
- Upper extremity fracture fixation in non-load-bearing applications
- Ankle fracture fixation in patients with metal allergies

How Do Manufacturing Processes Affect Ceramic Implant Performance?
The manufacturing pathway for advanced ceramic implants significantly influences their clinical performance, with each production step affecting the final material properties.
The production details you rarely hear about determine much of an implant’s success or failure. From powder preparation to final sintering, each manufacturing decision impacts the microstructure and performance of ceramic materials.
The typical manufacturing sequence includes:
| Manufacturing Stage | Process Parameters | Impact on Properties |
|---|---|---|
| Powder preparation | Particle size: 0.1-0.6 μm Purity: >99.9% | Affects density, grain size, and strength |
| Forming/pressing | Pressure: 100-300 MPa Binder content: 2-5% | Determines green body homogeneity |
| Pre-sintering | Temperature: 900-1100°C Duration: 1-2 hours | Creates machinable state |
| Machining | Tool type: Diamond-coated Cooling: Continuous | Introduces surface defects |
| Final sintering | Temperature: 1350-1550°C Duration: 2-4 hours Atmosphere: Air or inert gas | Determines final density, grain size, phase composition |
| Surface treatment | Methods: Sandblasting, acid etching, laser modification | Affects osseointegration and strength |
Powder characteristics play a crucial role in the final product quality. Nanoscale powders (particle size <100 nm) produce finer grain structures with improved mechanical properties compared to conventional powders. Studies show that reducing the starting particle size from 0.5 μm to 0.1 μm can increase flexural strength by 15-20%.
Sintering conditions dramatically affect phase stability of ceramic materials. Higher sintering temperatures produce larger grain sizes, which can reduce fracture toughness. The optimal sintering protocol balances density (ideally >99.5% of theoretical) with controlled grain growth (target grain size 0.3-0.5 μm).
Surface treatments create the critical interface that determines biological response. Common approaches include:
- Sandblasting with alumina particles (50-250 μm) creates micro-roughness that enhances osseointegration but may introduce surface flaws.
- Acid etching with hydrofluoric acid creates nanoscale roughness that promotes protein adsorption and cell attachment.
- Laser modification produces precise surface patterns that can be optimized for specific cell responses.
- Bioactive coatings such as hydroxyapatite or bioactive glass can accelerate bone formation but may have long-term stability concerns.
Quality control challenges are substantial for ceramic implants. Non-destructive testing methods such as X-ray computed tomography and acoustic microscopy can detect internal defects as small as 20-50 μm, but implementation across all production units remains challenging. The International Organization for Standardization has established specific standards (ISO 13356) for surgical implants made of yttria-stabilized tetragonal zirconia to ensure consistent quality.
Recent manufacturing innovations have addressed some historical limitations:
- Hot isostatic pressing (HIP) applies high pressure (100-200 MPa) and temperature simultaneously, eliminating residual porosity and increasing strength by 15-25%.
- Microwave sintering reduces processing time from hours to minutes while achieving more uniform densification.
- Additive manufacturing (3D printing) of ceramic materials, though still emerging, promises to enable complex geometries previously impossible with traditional methods.
- Hybrid materials that combine ceramic and metal components leverage the advantages of both while mitigating their respective limitations.
The economics of ceramic implant manufacturing continue to evolve. While production costs remain 30-50% higher than comparable titanium components, economies of scale and process refinements are gradually reducing this gap. The higher material cost is increasingly offset by improved clinical outcomes and reduced revision rates in appropriate applications.
Conclusion
The five key areas where zirconia outperforms titanium in orthopedic applications—material properties, patient outcomes, manufacturing capabilities, specific clinical applications, and long-term performance—demonstrate why this advanced ceramic has gained significant traction in modern orthopedic practice. While not suitable for every application, zirconia offers compelling advantages for specific patient populations and anatomical locations. As manufacturing techniques continue to advance and clinical experience grows, we can expect further refinement of indications and outcomes for this promising biomaterial.
FAQ
Q1: Are ceramic implants more expensive than titanium alternatives?
Yes, ceramic implants typically cost 30-50% more than comparable titanium components due to more complex manufacturing processes and higher material costs. However, this price differential has been decreasing as production volumes increase and manufacturing techniques improve. Many healthcare systems find the higher initial cost justified by improved clinical outcomes, reduced complication rates, and lower revision surgery frequency in appropriate applications.
Q2: How do ceramic implants perform in high-load applications like knee replacements?
Ceramic materials excel in compressive strength but have lower tensile strength and fracture toughness than titanium. For knee replacements, this means ceramic components perform exceptionally well for femoral components (primarily under compression) but may be less suitable for tibial components that experience more complex loading patterns. Modern designs often use ceramic selectively for articulating surfaces while maintaining titanium or cobalt-chromium for structural components.
Q3: What is the expected lifespan of a ceramic orthopedic implant?
Clinical data suggests ceramic implants can match or exceed the longevity of titanium implants in appropriate applications. Hip replacement studies show 10-year survival rates of 95-97% for ceramic femoral heads compared to 93-95% for titanium. The primary advantage comes from reduced wear rates and lower incidence of aseptic loosening. However, ceramic implant longevity depends heavily on proper patient selection, surgical technique, and implant design.
Q4: Can ceramic implants be revised if necessary?
Revision of ceramic implants presents unique challenges compared to titanium. The material cannot be cut or drilled intraoperatively like metal, requiring special extraction techniques. Complete removal is often necessary rather than partial revision. However, the biological advantages of ceramics, including reduced tissue staining and inflammatory response, can make the revision site more favorable. Surgeons should be specifically trained in ceramic implant revision techniques.
Q5: Are ceramic implants suitable for patients with osteoporosis?
Ceramic implants require careful consideration in patients with compromised bone quality. The higher stiffness (elastic modulus) of ceramic materials compared to titanium can increase stress shielding and potentially accelerate bone loss in osteoporotic patients. However, the excellent biocompatibility and reduced inflammatory response may benefit this population. Current best practice suggests using ceramic components selectively (such as for articulating surfaces) while maintaining titanium for bone-interfacing components in osteoporotic patients.